Intake to Follow-Up Pipeline
Create a complete prompt pipeline for the patient journey—from first visit through treatment to follow-up, with consistent documentation at every step.
A patient visits your clinic. They register, see you, get prescriptions, and leave. Three weeks later, they return—but can you quickly recall what happened, what you advised, and what needed follow-up? This article shows you how to create a complete prompt pipeline that tracks every patient from first contact through follow-up, ensuring nothing falls through the cracks.
What Problem This Solves
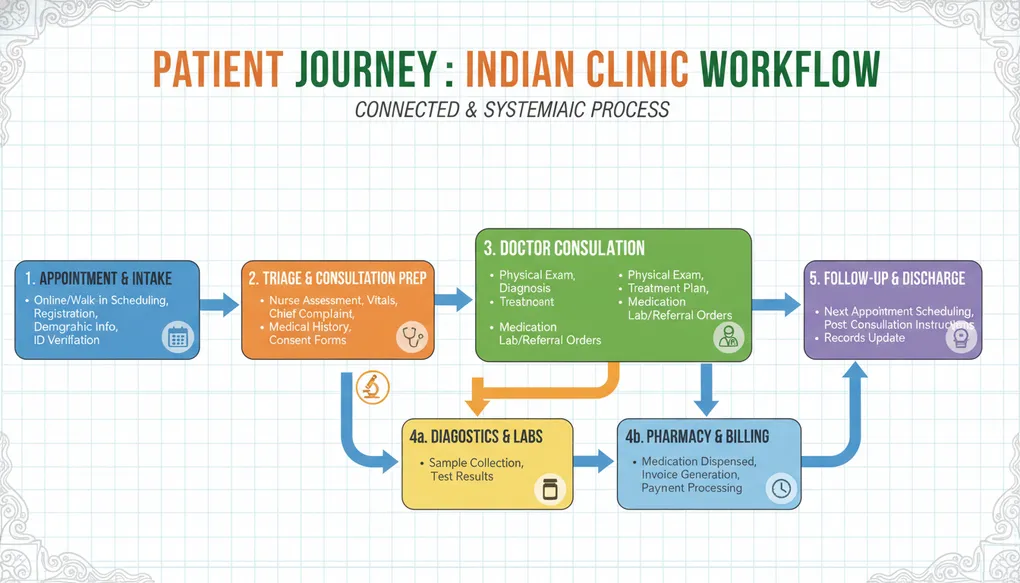
In busy Indian clinics, patient care happens in stages: the receptionist handles intake, you conduct the consultation, your assistant provides instructions, and someone needs to track follow-ups. Information gets lost at every handoff. The patient forgets what you said. Your notes are rushed. Follow-up calls don’t happen.
A prompt pipeline solves this by creating connected prompts for each stage of the patient journey. Each stage’s output feeds into the next, creating a complete, traceable record. No more asking “What did we discuss last time?” or “Did anyone call this patient for their blood test results?”
This builds on what you learned in D1 (SOAP notes), D2 (patient explanations), D3 (treatment plans), and E1 (medical translation)—now connecting them into one seamless workflow.
How to Do It (Steps)
Step 1: Map Your Clinic’s Patient Flow
Before creating prompts, understand your specific workflow:
- Who handles registration?
- How does information reach you before consultation?
- Who gives post-visit instructions?
- How are follow-ups tracked?
Step 2: Create Stage-Specific Prompts
Design prompts for each stage that:
- Take input from the previous stage
- Produce output the next stage needs
- Include patient identifiers for tracking
Step 3: Establish Handoff Points
Define what information must transfer between stages:
- Pre-visit to Intake: appointment type, special preparations
- Intake to Consultation: demographics, chief complaint, vitals
- Consultation to Post-visit: diagnosis, instructions, prescriptions
- Post-visit to Follow-up: what to track, when to call
Step 4: Build Tracking Mechanisms
Include prompts that:
- Generate follow-up task lists
- Create reminder messages
- Summarize patient status for next visit
Step 5: Test the Complete Pipeline
Run a sample patient through all stages to ensure:
- No information gaps
- Each stage has what it needs
- Follow-ups are captured
Example Prompts
Stage 1: Pre-Visit (Appointment Confirmation)
Generate an appointment confirmation message for:
Patient: [PATIENT NAME]
Appointment: [DATE] at [TIME]
Doctor: [YOUR NAME]
Clinic: [CLINIC NAME AND ADDRESS]
Visit Type: [NEW PATIENT / FOLLOW-UP / SPECIFIC PROCEDURE]
Include:
1. Confirmation of date, time, location
2. Documents to bring (Aadhaar, previous reports, current medications list)
3. Specific preparations if any: [FASTING REQUIRED / STOP CERTAIN MEDICATIONS / NONE]
4. Arrival time (15 minutes before appointment)
5. Cancellation/rescheduling instructions
6. Clinic contact number: [PHONE]
Language: [ENGLISH / HINDI / SPECIFY]
Tone: Friendly but professional
End with a reminder to bring all current medication strips/bottles.Stage 2: Intake (Chief Complaint Capture)
Convert this intake information into a structured pre-consultation summary:
Patient Details:
- Name: [NAME]
- Age: [AGE], Gender: [M/F]
- Phone: [NUMBER]
- Address: [LOCALITY/AREA]
Visit Information:
- Date: [TODAY'S DATE]
- Visit Type: [NEW / FOLLOW-UP FROM DATE]
- Referred by: [SELF / DR NAME / OTHER]
Chief Complaint (as stated by patient):
"[PATIENT'S EXACT WORDS ABOUT WHY THEY CAME]"
Vitals Recorded:
- BP: [SYSTOLIC/DIASTOLIC] mmHg
- Pulse: [RATE] /min
- Temperature: [TEMP] F
- Weight: [KG]
- SpO2: [PERCENTAGE]% (if recorded)
Current Medications (from strips/bottles brought):
[LIST MEDICATIONS PATIENT IS TAKING]
Allergies Mentioned: [ANY / NONE KNOWN]
Previous Reports Brought: [YES - LIST TYPES / NO]
Format this as a quick-reference summary I can review in 30 seconds before the patient enters my consultation room. Highlight anything concerning in the vitals or chief complaint.Stage 3: Consultation (SOAP Note Generation)
Generate a SOAP note from this consultation:
Patient: [NAME], [AGE] [GENDER]
Visit Date: [DATE]
Visit Type: [NEW CONSULTATION / FOLLOW-UP]
Pre-consultation summary:
[PASTE OUTPUT FROM INTAKE STAGE]
My clinical findings and observations:
[YOUR EXAMINATION FINDINGS AND CLINICAL NOTES]
Assessment:
[YOUR DIAGNOSIS OR DIFFERENTIAL DIAGNOSES]
Plan decided:
[INVESTIGATIONS ORDERED, MEDICATIONS PRESCRIBED, ADVICE GIVEN]
Create a complete SOAP note that:
1. Incorporates the intake information appropriately
2. Documents my examination findings
3. Records assessment and plan
4. Flags items needing follow-up
5. Notes what patient education was provided
At the end, generate a "Handoff Summary" section with:
- Key points for post-visit instructions
- Follow-up requirements (when, what to check)
- Red flags patient should watch forStage 4: Post-Visit (Patient Instructions)
Create patient take-home instructions based on this consultation:
Consultation Summary:
[PASTE HANDOFF SUMMARY FROM SOAP NOTE]
Prescriptions Given:
[LIST ALL MEDICATIONS WITH DOSES]
Generate instructions in [HINDI / ENGLISH / SIMPLE ENGLISH]:
Include:
1. Diagnosis explanation in simple terms (2-3 sentences)
2. Medication schedule in table format:
- Medicine name (with color/size description if possible)
- When to take (morning/afternoon/night, before/after food)
- For how many days
- Special instructions
3. Lifestyle advice specific to condition
4. Warning signs requiring immediate attention
5. What to do if warning signs appear
6. Follow-up appointment: [DATE/TIMEFRAME]
7. Reports to get before follow-up: [LIST ANY]
Format for easy reading. Use bullet points.
Include clinic contact number for emergencies: [NUMBER]Stage 5: Follow-Up (Progress Tracking)
Generate a follow-up tracking summary and patient contact message:
Patient: [NAME]
Original Visit: [DATE]
Diagnosis: [DIAGNOSIS]
Treatment Started: [MEDICATIONS/INTERVENTIONS]
Follow-up Due: [DATE]
Information from original consultation:
[PASTE RELEVANT SECTIONS FROM SOAP NOTE]
Tasks:
1. Create a follow-up call script for my staff to use 1-2 days before the appointment:
- Reminder about appointment
- Check if patient got tests done
- Ask about medication compliance
- Note any new symptoms to inform me
2. Create a pre-visit summary for me showing:
- Why patient originally came
- What we found and prescribed
- What improvement we expected
- What tests were ordered
- Key things to check this visit
3. Generate questions I should ask at follow-up
Language for patient contact: [HINDI / ENGLISH]Bad Prompt vs Improved Prompt
Bad Prompt:
Help me manage my patients from start to finish.Why it fails: No structure, no specific information, no clear stages or outputs needed.
Improved Prompt:
I'm setting up a patient tracking system for my ENT clinic in Pune. Create a prompt template for Stage 2 (Intake) that my receptionist can fill in.
The template should capture:
- Patient demographics (name, age, gender, contact, address)
- Chief complaint in patient's own words
- Vitals (BP, pulse, weight)
- Current medications (from strips they bring)
- Previous ENT history if any
- Insurance/payment mode
Output should be a structured summary I can review in under 1 minute before consultation. Highlight any red flags (very high BP, concerning symptoms like sudden hearing loss or facial weakness).
Format should work when copy-pasted into WhatsApp (my staff sends me summaries there).Why it works: Specifies the exact stage, what information to capture, desired output format, practical constraints (WhatsApp-compatible), and specialty context.
Common Mistakes
1. Creating Isolated Prompts Each prompt works alone but doesn’t connect to others. The consultation prompt doesn’t use intake data; follow-up prompt doesn’t reference original findings.
Fix: Always include a section for input from the previous stage and output for the next stage.
2. Inconsistent Patient Identifiers Intake uses patient name, consultation uses file number, follow-up uses phone number. Nothing links together.
Fix: Standardize identifiers across all stages. At minimum: Name + Phone + Visit Date.
3. Missing Handoff Information Consultation note doesn’t specify what follow-up is needed. Staff don’t know who needs callbacks.
Fix: Every consultation output should include explicit follow-up requirements.
4. Language Inconsistency Intake in English, instructions in Hindi, follow-up calls in English. Patient gets confused.
Fix: Note patient’s preferred language at intake, use it consistently.
5. No Red Flag Escalation Pipeline handles routine cases but doesn’t flag urgent situations differently.
Fix: Include urgency assessment at each stage with clear escalation paths.
6. Overcomplicating for Staff Prompts require medical knowledge your receptionist doesn’t have.
Fix: Stage-appropriate prompts. Reception prompts should need no medical interpretation.
Clinic-Ready Templates
Complete Pipeline Checklist Template
PATIENT PIPELINE TRACKING SHEET
================================
Patient: _________________ Phone: _________________
Date: _________________ File #: _________________
STAGE 1: PRE-VISIT [ ]
- Appointment confirmed: [ ] Yes [ ] No
- Preparation instructions sent: [ ] Yes [ ] N/A
- Documents reminder sent: [ ] Yes [ ] No
- Notes: _________________________________
STAGE 2: INTAKE [ ]
- Registration complete: [ ] Yes
- Chief complaint recorded: [ ] Yes
- Vitals taken: [ ] Yes
- Current medications listed: [ ] Yes
- Previous reports collected: [ ] Yes [ ] None brought
- Pre-consultation summary sent to doctor: [ ] Yes
- Red flags identified: [ ] None [ ] Yes: ___________
STAGE 3: CONSULTATION [ ]
- SOAP note completed: [ ] Yes
- Prescriptions written: [ ] Yes
- Investigations ordered: [ ] Yes [ ] None needed
- Patient education provided: [ ] Yes
- Follow-up plan documented: [ ] Yes
- Handoff summary prepared: [ ] Yes
STAGE 4: POST-VISIT [ ]
- Instructions explained: [ ] Yes
- Written instructions given: [ ] Yes
- Prescription explained: [ ] Yes
- Warning signs explained: [ ] Yes
- Follow-up appointment: Date: _______ [ ] Booked [ ] Patient will call
- Tests to do before follow-up: ____________
STAGE 5: FOLLOW-UP TRACKING [ ]
- Added to follow-up calendar: [ ] Yes
- Reminder call scheduled for: _____________
- Reminder call completed: [ ] Yes [ ] No answer [ ] Rescheduled
- Test results received: [ ] Yes [ ] No [ ] N/A
- Patient showed for follow-up: [ ] Yes [ ] No-show [ ] Rescheduled
NOTES/ISSUES:
_________________________________________________Multi-Patient Daily Follow-Up Tracker Prompt
Create a daily follow-up task list from these patient records:
Today's Date: [DATE]
Patients needing follow-up:
[PASTE LIST WITH: Name, Phone, Original Visit Date, Reason for Follow-up]
For each patient, generate:
1. Priority level (High/Medium/Low based on condition)
2. Suggested call time (morning for elderly, afternoon for working adults)
3. Key questions to ask
4. Action based on response (reschedule/note symptoms/confirm visit)
Format as a checklist my staff can print and tick off.
Group by priority, then by suggested call time.
Add a summary row at top: Total calls, High priority count, Overdue follow-ups.Stage Handoff Template
HANDOFF: [FROM STAGE] → [TO STAGE]
===================================
Patient: [NAME]
Date: [DATE]
Completed by: [STAFF NAME/ROLE]
SUMMARY OF COMPLETED STAGE:
[Key information from the stage just finished]
FOR NEXT STAGE - REQUIRED ACTIONS:
1. [Action item]
2. [Action item]
3. [Action item]
CRITICAL INFORMATION:
- Allergies: [LIST/NONE]
- Red Flags: [LIST/NONE]
- Special Needs: [LANGUAGE/MOBILITY/OTHER]
PENDING ITEMS:
- [Anything incomplete that next stage should know]
FOLLOW-UP REQUIREMENTS:
- [What needs to be tracked/scheduled]Safety Note
Pipeline limitations you must remember:
-
AI doesn’t replace clinical judgment: Every stage involving medical decisions requires your review. AI helps organize and format, not diagnose or prescribe.
-
Emergencies bypass the pipeline: A patient with chest pain doesn’t wait for Stage 2 documentation. Train staff on red flags that skip directly to clinical attention.
-
Data security: Patient information in prompts goes to AI servers. Use initials or codes for sensitive cases. Never include Aadhaar numbers, full addresses, or financial details in prompts.
-
Verify before sending: Any AI-generated patient communication must be reviewed before sending. One wrong instruction can cause harm.
-
Pipeline is not EMR: This system helps with documentation but doesn’t replace proper medical records. Maintain your official records as required by law.
-
Follow-up is clinical, not just administrative: If a patient misses follow-up for a serious condition, that’s a clinical concern, not just a scheduling issue. Build escalation into your pipeline.
Copy-Paste Prompts
Quick Pre-Visit Confirmation Generator
Create an appointment reminder SMS (under 160 characters) for:
Patient: [NAME]
Doctor: Dr. [YOUR NAME]
Date: [DATE], Time: [TIME]
Clinic: [CLINIC NAME]
Special instruction: [FASTING/BRING REPORTS/NONE]
Language: [HINDI/ENGLISH]
Include: Date, time, one key preparation point, clinic phone.Rapid Intake Summary
Quick intake summary for doctor:
Patient: [NAME], [AGE][M/F]
Complaint: "[PATIENT'S WORDS]"
Duration: [HOW LONG]
Vitals: BP [X/Y], Pulse [Z], Wt [KG]
Meds: [CURRENT MEDICATIONS]
Allergy: [Y/N - WHAT]
Reports brought: [Y/N - WHICH]
Flag if: BP>160 or <90, Pulse>100 or <60, concerning symptoms
Format: 5 lines maximum, ready to read in 30 seconds.Post-Consultation Quick Instructions
Simple take-home instructions for [CONDITION]:
Medicines:
[LIST: MEDICINE - DOSE - TIMING]
Generate in [HINDI/ENGLISH]:
1. When to take each medicine (use breakfast/lunch/dinner, not medical timing)
2. What to avoid (food/activities)
3. One key warning sign to watch
4. When to return or call
Keep under 10 lines. Patient is [ELDERLY/ADULT/PARENT OF CHILD].Follow-Up Call Script
Phone script for follow-up call:
Patient: [NAME]
Visited: [DATE] for [CONDITION]
Treatment: [MAIN MEDICATIONS]
Follow-up due: [DATE]
Create a friendly script in [HINDI/ENGLISH] for my staff:
1. Greeting and identification
2. Reminder about follow-up date
3. Questions about: medication compliance, symptom improvement, any new problems
4. What to note based on answers
5. Closing with next steps
Keep conversational. Include prompts for common patient responses.End-of-Day Follow-Up Summary
Create tomorrow's follow-up priority list:
Patients due for follow-up:
[PASTE: NAME | PHONE | LAST VISIT | CONDITION | WHAT TO CHECK]
Categorize by:
- URGENT (chronic conditions, elderly, post-procedure)
- ROUTINE (stable conditions, young adults)
- FLEXIBLE (can wait few more days if busy)
For each, give:
- Best time to call
- Key question to ask
- Action if no answer
Format as printable checklist.Do’s and Don’ts
Do’s
Do standardize your pipeline for your clinic’s specific workflow. What works for a solo GP differs from a multi-doctor specialty clinic.
Do train all staff on their stage responsibilities. Receptionist handles intake prompts, assistant handles post-visit prompts. Clear ownership prevents gaps.
Do include patient language preference at intake. Use it consistently through all stages.
Do build in checkpoints. Before patient leaves, verify: instructions given, follow-up scheduled, contact number confirmed.
Do review AI outputs before use. Especially patient-facing communications and clinical summaries.
Do keep templates updated. When you notice gaps or errors, improve the prompts.
Do use the pipeline for learning. Review completed pipelines to see where care could improve.
Don’ts
Don’t make the pipeline more important than the patient. If documentation slows urgent care, care comes first.
Don’t assume AI understands medical urgency. A complaint of “chest pain since 5 minutes” needs immediate attention, not documentation.
Don’t include unnecessary personal details in prompts. Use minimum information needed for the task.
Don’t skip stages for “simple” cases. The diabetic coming for “just a refill” still needs proper documentation and follow-up.
Don’t let follow-ups go untracked. An untreated patient is worse than an undocumented one.
Don’t use one-size-fits-all templates. Pediatric intake differs from geriatric. Customize.
Don’t forget the human element. Pipeline helps organization, but patient rapport happens in person.
1-Minute Takeaway
The patient journey pipeline in 60 seconds:
Five stages, five connected prompts:
- Pre-visit: Confirm appointment, send preparation instructions
- Intake: Capture demographics, complaints, vitals, current medications
- Consultation: Generate SOAP note with handoff summary for next stage
- Post-visit: Create simple instructions patient can follow at home
- Follow-up: Track who needs callbacks, prepare for their return visit
The key principle: Each stage’s output feeds the next stage’s input. Nothing gets lost.
Quick implementation:
- Start with intake and post-visit prompts (highest impact)
- Add follow-up tracking next (prevents patients falling through cracks)
- Build pre-visit automation last (nice-to-have)
Daily habit: End each day by reviewing the follow-up list. One minute of prevention saves hours of emergency management.
Remember: The pipeline serves the patient, not the other way around. When in doubt, talk to the patient. Technology supports care; it doesn’t replace it.