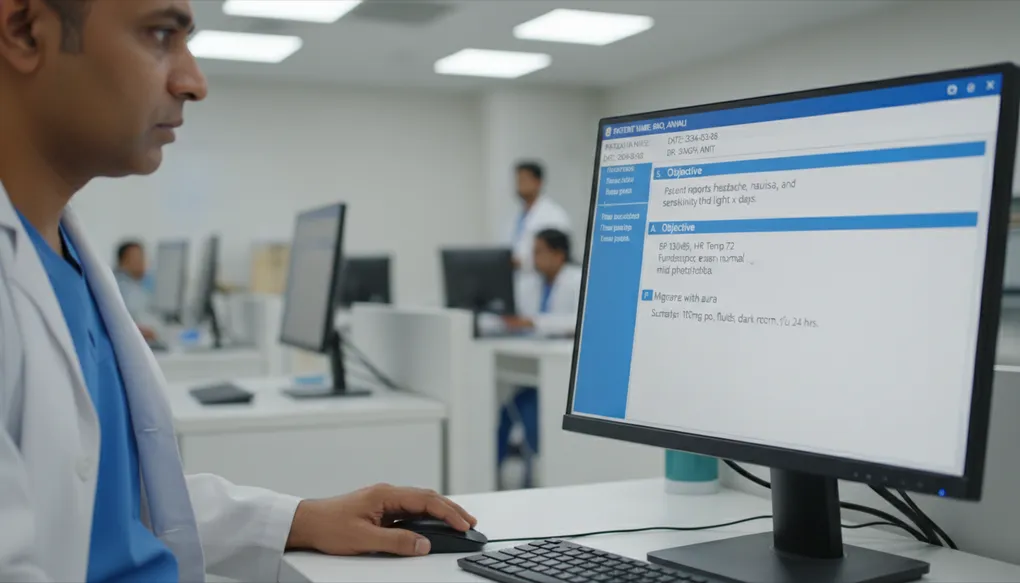
SOAP and EMR Note Drafting
Draft professional SOAP notes and EMR entries quickly—maintain documentation standards while saving time during busy clinic hours.
It is 2 PM. You have seen 28 patients since morning. Your EMR shows 12 incomplete notes from yesterday. The hospital administrator sends another reminder about documentation compliance. Your hand hovers over the keyboard, but you cannot recall the exact sequence of that third patient’s presenting complaints.
Sound familiar? Clinical documentation is essential for patient safety, continuity of care, and medico-legal protection. But writing detailed SOAP notes while managing a packed OPD feels impossible. Most Indian doctors either rush through documentation (creating incomplete records) or stay late completing notes (adding to burnout).
This article shows you how to use AI to draft professional SOAP notes and EMR entries in seconds—while you retain full control over the clinical content.
Remember: AI drafts, you review and sign. The final note is always your professional responsibility.
What Problem This Solves
Documentation burdens are crushing Indian clinicians:
The Time Problem
- A well-documented SOAP note takes 5-8 minutes to write properly
- Multiply by 40-60 patients daily, and documentation alone could take 4-8 hours
- Reality: most doctors have 2-3 minutes maximum per patient encounter
- Result: incomplete notes, missed details, medicolegal vulnerability
The Quality Problem
- Rushed notes miss critical information
- Inconsistent formats make records hard to review
- Handwritten notes in many clinics remain illegible
- EMR systems often have rigid templates that do not fit actual workflow
The Compliance Problem
- NABH accreditation requires specific documentation standards
- Insurance claims get rejected for incomplete records
- Medico-legal cases increasingly scrutinise documentation quality
- Audit findings cite documentation gaps as top deficiencies
What AI Documentation Assistance Solves:
- Reduces note-writing time by 60-70%
- Ensures consistent structure and completeness
- Catches missing elements before finalisation
- Frees cognitive load for clinical thinking during the encounter
- Creates a draft you can quickly review and approve
Important: This builds on the 5-Part Prompt Formula (Article B1) for structuring your requests, and follows the Medico-Legal Safe Drafting principles (Article C2) for documentation that protects you.
How to Do It (Steps)
Step 1: Capture Key Information During the Encounter
Do not try to dictate a full note while with the patient. Instead, capture essential elements:
- Chief complaint (in patient’s words)
- Key history points
- Relevant examination findings
- Your working impression
- Plan elements
You can jot these on paper, type quick bullet points, or use voice notes between patients.
Step 2: De-Identify Before Prompting
Before using AI, remove or replace:
- Patient name (use “Patient” or initials)
- Specific dates of birth (use age only)
- Phone numbers and addresses
- Aadhaar or insurance numbers
- Hospital registration numbers
Example of de-identification:
- Original: “Ramesh Sharma, 45M, DOB 15-08-1980, Mob: 9876543210”
- De-identified: “45-year-old male”
Step 3: Structure Your Prompt Using the SOAP Framework
Use this basic structure for your prompts:
Act as a medical documentation assistant familiar with Indian clinical practice.
Convert the following clinical information into a SOAP note format.
Patient: [AGE]-year-old [GENDER]
Presenting complaint: [CHIEF COMPLAINT]
History: [KEY HISTORY POINTS]
Examination: [RELEVANT FINDINGS]
Impression: [YOUR WORKING ASSESSMENT]
Plan: [INTENDED MANAGEMENT]
Constraints:
- Do not add clinical information not provided
- List assessment as "Working Assessment" or "Clinical Impression"
- Use standard medical terminology
- Mark missing information as [TO BE ADDED]
- Keep note concise but completeStep 4: Choose Your Note Type
Different encounters need different documentation approaches:
Initial Consultation (New Patient):
- Detailed history including past medical, family, social history
- Complete review of systems
- Comprehensive examination
- Differential considerations
Follow-Up Visit:
- Brief interval history
- Relevant examination changes
- Response to treatment
- Plan modifications
Urgent/Acute Visit:
- Focused complaint-based history
- Targeted examination
- Red flag assessment
- Immediate management plan
Step 5: Review, Edit, and Sign
This is non-negotiable. Every AI-generated note must be:
- Read completely
- Verified against your clinical encounter
- Modified based on your judgment
- Signed as your professional document
Example Prompts
Example 1: Initial Consultation SOAP Note
Act as a medical documentation assistant for an Indian outpatient clinic.
Convert this into a complete initial consultation SOAP note:
Patient: 52-year-old female, homemaker
Chief Complaint: Knee pain bilateral, 6 months, worse on stairs
History: Gradual onset, no trauma, morning stiffness 20 min, improves with movement, OTC painkillers give partial relief, no swelling noticed
Past Medical: Type 2 DM for 8 years (on Metformin 500 BD), HTN 3 years (Telmisartan 40 OD)
No surgical history, no allergies
Family: Mother had knee replacement
Examination: BMI 28, bilateral knee crepitus, no effusion, ROM full but painful terminal flexion, varus alignment noted, tenderness medial joint line bilateral
X-ray done today: Bilateral knee OA Grade 2 KL
Format: Standard SOAP with separate sections clearly labelled
Include: Assessment with staging, Plan with medications placeholder, lifestyle advice, follow-up planExample 2: Follow-Up Visit (Diabetes Review)
Act as a medical documentation assistant.
Create a follow-up SOAP note for:
Patient: 58-year-old male, known T2DM for 12 years
Visit type: 3-month diabetes review
Current Medications: Metformin 1000 BD, Glimepiride 2mg OD, Atorvastatin 10 OD
Today's readings: FBS 142, PPBS 198, HbA1c 7.8% (previous 8.2%)
BP: 136/84
Weight: 78 kg (previous 80 kg)
Symptoms: No hypoglycemia, occasional tingling feet (unchanged)
Foot exam: Normal
Fundus: Last checked 4 months ago, normal
Patient reports: Better diet compliance, walking 20 min daily
Concerns: Wants to know if medicines can be reduced
Plan: Continue current medications, reinforce lifestyle, recheck HbA1c in 3 months, annual eye check due
Keep note concise, appropriate for EMR entry.Example 3: Urgent Visit (Acute Presentation)
Medical documentation assistant - create an urgent visit SOAP note:
Patient: 35-year-old male, software professional
Presented with: Severe headache since yesterday evening
Character: Throbbing, bilateral temporal, 8/10 severity
Associated: Nausea (no vomiting), photophobia, missed lunch and dinner yesterday
No fever, no neck stiffness, no visual changes, no weakness
No history of head injury, no similar episodes before
PMH: Nil significant, no regular medications
Examination: Afebrile, BP 124/80, neurologically intact, no meningeal signs, no papilledema on fundoscopy
Impression: Likely severe migraine vs tension-type headache, first episode
Plan: Symptomatic relief, hydration, advised rest, red flags explained, review if worsening or new symptoms
Format: Focused SOAP appropriate for acute care documentation
Include red flag counselling in planExample 4: Procedure Documentation (Minor Procedure)
Create a procedure note for Indian outpatient setting:
Procedure: Incision and drainage of abscess
Location: Right gluteal region
Patient: 42-year-old male, diabetic
Indication: Gluteal abscess not responding to antibiotics x 5 days
Procedure details:
- Informed consent obtained
- Area cleaned with povidone-iodine
- Local anesthesia: 2% lignocaine 5ml infiltrated
- Cruciate incision made
- Approximately 15ml pus drained
- Cavity irrigated with saline
- Gauze wick placed
- Sterile dressing applied
- Sample sent for culture sensitivity
Complications: None
Post-procedure: Stable, wound care instructions given
Follow-up: Dressing change after 48 hours
Format: Standard procedure note with all medicolegal elementsExample 5: EMR-Compatible Quick Note
Format this into a brief EMR-compatible clinic note (Indian hospital system):
45M, shopkeeper
C/O: Cough 2 weeks, mild fever evenings
H/O: Dry cough, no hemoptysis, low-grade fever evenings, night sweats +, appetite reduced, weight loss noticed (not measured)
Smoker 10 pack years, quit 2 years ago
No known TB contact, no diabetes
O/E: Thin built, no lymphadenopathy, chest - reduced breath sounds right upper zone, no added sounds
Temp: 99.2F, SpO2: 97% RA
Impression: Suspected PTB, needs workup
Advised: CXR, sputum AFB x 2, CBC, ESR, RBS
Return with reports in 3 days
Format: Compact clinical note suitable for hospital EMR, include ICD considerationBad Prompt → Improved Prompt
Bad Prompt:
Write a SOAP note for my diabetic patient.What is wrong:
- No patient details provided
- No clinical findings mentioned
- No context about visit type
- No specific instructions about format needed
- AI will generate generic content that is useless
Improved Prompt:
Act as a medical documentation assistant for an Indian diabetology clinic.
Create a SOAP note for:
Patient: 62-year-old female, retired teacher
Visit Type: Quarterly diabetes review
Duration of Diabetes: 15 years, on insulin for 5 years
Subjective Data:
- No hypoglycemic episodes
- Occasional numbness in feet, unchanged
- Compliance: admits missing evening insulin sometimes
- Diet: "trying to follow"
- Exercise: walks 15 minutes daily
Objective Data:
- Weight: 68 kg (stable)
- BP: 138/86
- HbA1c: 8.4% (previous: 8.1% three months ago)
- Fasting sugar today: 156 mg/dL
- Creatinine: 1.1 (eGFR 62)
- Urine ACR: 45 mg/g
- Foot exam: diminished sensation monofilament test, pulses present
- Current medications: Metformin 1000 BD, Insulin Glargine 20u HS, Insulin Aspart 8-8-8 AC meals
Constraints:
- Use standard SOAP format
- Include specific assessment addressing glycemic control, nephropathy status, neuropathy
- Plan should address: insulin adjustment consideration, nephropathy management, neuropathy monitoring
- Note any missing information as [TO BE CONFIRMED]
- Keep professional tone appropriate for hospital records
Format: Structured SOAP with clearly labelled sectionsWhy this is better:
- Complete patient information provided
- Specific clinical data included
- Clear format instructions
- Appropriate constraints for medical documentation
- Allows AI to produce a useful, verifiable draft
Common Mistakes
Mistake 1: Including Patient Identifiers
Problem: Pasting full patient details including name, phone, Aadhaar into AI prompts Fix: Always de-identify. Use age, gender, and occupation only. Never include unique identifiers.
Mistake 2: Asking AI to Add Clinical Findings
Problem: “Make the examination more complete” or “Add appropriate findings” Fix: AI should only structure what you provide. Fabricated clinical findings are dangerous and potentially fraudulent.
Mistake 3: Using AI-Suggested Diagnoses as Final
Problem: AI writes “Diagnosis: Rheumatoid Arthritis” and you accept it without your own clinical reasoning Fix: Instruct AI to use “Working Impression” or “Clinical Considerations.” The diagnosis is always your professional conclusion.
Mistake 4: Skipping Review Because Note “Looks Correct”
Problem: The note appears professional, so you sign without reading carefully Fix: Read every word. AI can hallucinate medications, contradict your actual findings, or include inappropriate recommendations.
Mistake 5: Using Same Template for All Visit Types
Problem: Using a detailed initial consultation template for a quick follow-up Fix: Match documentation depth to encounter type. Follow-ups need focused notes, not comprehensive histories.
Mistake 6: Not Specifying Indian Clinical Context
Problem: Generic prompts produce notes with non-Indian drug names, unfamiliar formats, irrelevant recommendations Fix: Explicitly mention “Indian clinical practice,” use Indian brand names if needed, specify local EMR formats.
Clinic-Ready Templates
Template 1: Initial Consultation SOAP Note
Act as a medical documentation assistant for Indian outpatient practice.
Create an initial consultation SOAP note:
PATIENT INFORMATION:
- Age/Gender: [AGE]-year-old [MALE/FEMALE]
- Occupation: [OCCUPATION]
SUBJECTIVE:
- Chief Complaint: [MAIN COMPLAINT] for [DURATION]
- History of Present Illness: [DETAILED HPI]
- Past Medical History: [CONDITIONS AND DURATION]
- Past Surgical History: [SURGERIES WITH YEAR]
- Medications: [CURRENT MEDICATIONS WITH DOSES]
- Allergies: [KNOWN ALLERGIES OR NKDA]
- Family History: [RELEVANT FAMILY HISTORY]
- Social History: [SMOKING/ALCOHOL/OCCUPATION RELEVANT]
OBJECTIVE:
- Vitals: [BP, PULSE, TEMP, SPO2, WEIGHT, HEIGHT]
- General Examination: [GENERAL APPEARANCE, BUILD]
- Systemic Examination: [RELEVANT SYSTEMS EXAMINED]
- Investigations: [ANY TESTS DONE WITH RESULTS]
CLINICAL IMPRESSION: [YOUR WORKING DIAGNOSIS]
PLAN: [INTENDED MANAGEMENT]
Format Requirements:
- Use standard SOAP structure with clear section headers
- Assessment should include differential considerations if applicable
- Plan should include: medications (leave dosage for doctor), investigations needed, lifestyle advice, follow-up timeline, red flags counselled
- Mark any missing information as [PENDING]
- Professional language appropriate for hospital recordsTemplate 2: Follow-Up Visit Template
Medical documentation assistant - follow-up visit note:
Patient: [AGE]-year-old [GENDER]
Condition Being Followed: [PRIMARY CONDITION]
Last Visit: [APPROXIMATE TIME]
INTERVAL HISTORY:
- Symptoms since last visit: [CHANGES/IMPROVEMENTS/WORSENING]
- Medication compliance: [COMPLIANT/PARTIAL/NON-COMPLIANT]
- Side effects reported: [ANY SIDE EFFECTS]
- Patient concerns: [CURRENT CONCERNS]
TODAY'S FINDINGS:
- Vitals: [RELEVANT VITALS]
- Examination: [FOCUSED EXAMINATION RELEVANT TO CONDITION]
- Investigations reviewed: [RECENT TEST RESULTS]
ASSESSMENT: [CURRENT STATUS OF CONDITION - CONTROLLED/UNCONTROLLED/IMPROVING]
PLAN:
- Medication changes: [ANY MODIFICATIONS]
- Advice given: [COUNSELLING POINTS]
- Next review: [FOLLOW-UP TIMING]
Format: Concise follow-up note suitable for EMR entryTemplate 3: Urgent/Acute Visit Template
Create an acute visit SOAP note:
Patient: [AGE]-year-old [GENDER]
Presenting Complaint: [ACUTE COMPLAINT]
Duration: [ONSET AND DURATION]
FOCUSED HISTORY:
- Symptom details: [CHARACTER, SEVERITY, LOCATION, ASSOCIATED SYMPTOMS]
- Red flag symptoms: [PRESENCE OR ABSENCE OF RED FLAGS]
- Relevant past history: [PERTINENT PMH ONLY]
- Current medications: [RELEVANT MEDICATIONS]
EXAMINATION:
- General: [APPEARANCE, VITALS]
- Focused examination: [EXAMINATION RELEVANT TO COMPLAINT]
- Red flag signs: [ASSESSED AND DOCUMENTED]
ASSESSMENT: [CLINICAL IMPRESSION]
PLAN:
- Immediate management: [TREATMENT GIVEN/PRESCRIBED]
- Investigations: [IF ORDERED]
- Disposition: [DISCHARGE/REFER/ADMIT]
- Red flag counselling: [WARNING SIGNS EXPLAINED]
- Follow-up: [WHEN TO RETURN]
Include safety netting in plan section.Template 4: Progress Note (Inpatient)
Create an inpatient progress note (Indian hospital format):
Patient: [AGE]-year-old [GENDER]
Diagnosis: [ADMISSION DIAGNOSIS]
Day of Admission: Day [NUMBER]
SUBJECTIVE:
- Patient's current complaints: [TODAY'S SYMPTOMS]
- Sleep/appetite/bowel/bladder: [STATUS]
- Pain score: [IF APPLICABLE]
OBJECTIVE:
- General condition: [STABLE/IMPROVING/CRITICAL]
- Vitals: [TODAY'S VITALS]
- Systemic examination: [RELEVANT FINDINGS]
- Intake/Output: [IF MONITORING]
- Investigation results: [NEW RESULTS]
ASSESSMENT:
- Current status: [IMPRESSION OF PROGRESS]
- Active issues: [LIST ACTIVE PROBLEMS]
PLAN:
- Continue/Modify: [TREATMENT CHANGES]
- New orders: [ANY NEW INVESTIGATIONS OR TREATMENTS]
- Pending: [AWAITED RESULTS OR CONSULTATIONS]
- Anticipated course: [EXPECTED TRAJECTORY]
Format: Standard hospital progress noteSafety Note
Clinical Accountability Remains Yours
The Medical Council of India regulations are clear: the registered medical practitioner is responsible for all clinical documentation. AI-generated notes are drafts only. When you sign a note (physically or electronically), you are certifying its accuracy.
Documentation-Specific Safety Rules:
-
Never accept fabricated findings: If AI adds examination findings or history you did not obtain, delete them immediately. Fabricated documentation is both dangerous and potentially illegal.
-
Verify all medications: AI may suggest incorrect dosages, use non-Indian brand names, or miss contraindications. Always verify against your clinical judgment and patient-specific factors.
-
Assessment is your professional opinion: AI should provide structure, not conclusions. “Working impression” or “clinical considerations” are appropriate. “Diagnosis: X” should be your documented clinical conclusion.
-
De-identification is mandatory: Under the DPDP Act, 2023, sharing identifiable patient data with external AI systems violates data protection requirements. Always de-identify before prompting.
-
EMR audit trails: Most hospital EMRs log who created and edited notes. Ensure your AI-drafted notes are properly reviewed before final save. An unreviewed AI note entered into official records is your responsibility.
-
Timeliness matters: Document close to the encounter. AI can help you catch up, but “retrospective documentation” created days later raises medico-legal questions.
The Documentation Test: Would you be comfortable defending this note in a medical council inquiry or court? If not, revise it.
Copy-Paste Prompts
Prompt 1: Quick SOAP Note Generator
Act as a medical documentation assistant for Indian clinical practice.
Convert this into a SOAP note:
Patient: [AGE]-year-old [GENDER]
Chief Complaint: [COMPLAINT] for [DURATION]
Key History: [IMPORTANT HISTORY POINTS]
Examination: [RELEVANT FINDINGS]
Impression: [YOUR CLINICAL IMPRESSION]
Plan: [INTENDED MANAGEMENT]
Constraints:
- Use standard SOAP format
- Do not add information not provided
- Mark missing elements as [TO BE ADDED]
- Use "Working Assessment" not "Diagnosis"
- Keep professional and concisePrompt 2: Follow-Up Note (Quick Version)
Create a follow-up SOAP note:
Patient: [AGE]-year-old [GENDER] with [CONDITION]
Today's visit: [ROUTINE REVIEW/SYMPTOM CHANGE/TEST REVIEW]
Current symptoms: [STATUS - IMPROVED/SAME/WORSE]
Medications: [CURRENT LIST]
Today's findings: [VITALS, RELEVANT EXAM]
Recent investigations: [RESULTS IF ANY]
Plan: [CONTINUE/MODIFY/INVESTIGATE]
Format: Brief follow-up note for EMRPrompt 3: New Patient Comprehensive Note
Medical documentation assistant - create comprehensive initial consultation:
Demographics: [AGE, GENDER, OCCUPATION]
Chief Complaint: [MAIN ISSUE AND DURATION]
History:
- HPI: [DETAILED PRESENT ILLNESS]
- PMH: [PAST MEDICAL CONDITIONS]
- PSH: [SURGICAL HISTORY]
- Medications: [CURRENT DRUGS]
- Allergies: [KNOWN ALLERGIES]
- Family Hx: [RELEVANT FAMILY HISTORY]
- Social Hx: [SMOKING, ALCOHOL, OCCUPATION DETAILS]
Examination:
- Vitals: [ALL VITAL SIGNS]
- General: [GENERAL APPEARANCE]
- Systemic: [SYSTEM-WISE FINDINGS]
Investigations: [TESTS DONE WITH RESULTS]
My Impression: [YOUR WORKING ASSESSMENT]
My Plan: [INTENDED APPROACH]
Format: Complete SOAP with all sections clearly separated
Include differentials if applicable
Standard Indian hospital documentation formatPrompt 4: Procedure Note Template
Create a procedure note:
Procedure: [PROCEDURE NAME]
Date: [DATE]
Patient: [AGE, GENDER]
Indication: [WHY PROCEDURE WAS DONE]
Consent: [OBTAINED/TYPE OF CONSENT]
Procedure Details:
- Preparation: [CLEANING, POSITIONING]
- Anesthesia: [TYPE AND AMOUNT]
- Technique: [STEP-BY-STEP WHAT WAS DONE]
- Findings: [WHAT WAS FOUND]
- Complications: [NONE OR DESCRIBE]
Post-Procedure:
- Patient condition: [STABLE/OBSERVATION NEEDED]
- Instructions given: [CARE INSTRUCTIONS]
- Follow-up: [NEXT STEPS]
Format: Standard procedure documentation for medicolegal completenessPrompt 5: Discharge Summary Draft
Draft a discharge summary:
Patient: [AGE, GENDER, OCCUPATION]
Admission Date: [DATE]
Discharge Date: [DATE]
Admitting Diagnosis: [INITIAL DIAGNOSIS]
Final Diagnosis: [DISCHARGE DIAGNOSIS]
Hospital Course:
- Presenting complaint: [WHY ADMITTED]
- Key investigations: [IMPORTANT TESTS AND RESULTS]
- Treatment given: [MAIN TREATMENTS]
- Procedures: [IF ANY]
- Progress: [COURSE DURING STAY]
- Condition at discharge: [STATUS]
Discharge Medications: [LIST WITH DOSES]
Instructions: [DIET, ACTIVITY, WOUND CARE ETC]
Follow-up: [WHEN AND WHERE]
Warning Signs: [WHEN TO RETURN URGENTLY]
Format: Standard Indian hospital discharge summary
Include all sections required for insurance and recordsDo’s and Don’ts
Do’s
- Do capture clinical information during or immediately after the encounter
- Do de-identify all patient information before using AI tools
- Do use specific templates for different visit types (new, follow-up, urgent)
- Do read every word of AI-generated notes before signing
- Do verify that all clinical facts match your actual findings
- Do use “Working Assessment” or “Clinical Impression” rather than definitive diagnoses
- Do include constraints in your prompts to prevent AI overreach
- Do maintain your own clinical judgment as the final authority
- Do document close to the time of encounter for accuracy
- Do save effective prompts as templates for regular use
Don’ts
- Don’t include patient names, phone numbers, or identification numbers in prompts
- Don’t ask AI to add clinical findings you did not actually observe
- Don’t accept AI-suggested diagnoses without your own clinical reasoning
- Don’t skip the review step because the note “looks professional”
- Don’t use AI-generated notes as final documentation without verification
- Don’t let AI write prescriptions or specific dosages
- Don’t use the same detailed template for every visit type
- Don’t document encounters you did not personally conduct
- Don’t forget that medicolegal responsibility is entirely yours
- Don’t share AI-drafted notes with patients before your review
1-Minute Takeaway
The Documentation Problem: SOAP notes are essential but time-consuming. Most Indian doctors face a painful choice between thorough documentation and seeing enough patients.
The AI Solution: Use AI to draft structured notes from your clinical bullet points. This cuts documentation time by 60-70% while maintaining quality.
The Workflow:
- Capture key information during encounter
- De-identify patient data
- Use structured prompts for your note type
- Review and verify every word
- Sign as your professional document
The Golden Rules:
- AI structures and formats; you provide all clinical content
- Never ask AI to add findings or make diagnoses
- Always de-identify before prompting (DPDP Act, 2023)
- Review is mandatory, not optional
- Your signature means you verified everything
Remember: The best documentation is accurate, timely, and complete. AI helps you achieve all three without sacrificing your clinical time or burning out over paperwork.
Your notes, your responsibility, your signature. AI just helps you get there faster.
Next article: Consent and Procedure Note Drafting - creating clear, complete procedure documentation and consent checklists that protect both you and your patients.